Glucagon-like peptide-1 (GLP-1) agonists are a class of medications frequently used to treat type 2 diabetes mellitus (T2DM) and obesity.[1] This class of medications assists in lowering blood sugar levels and promotes weight loss. In addition to treating diabetics, these medications are also used to treat obesity in diabetics as well as non-diabetics. GLP-1 drugs can cost over $1,000 per month for treatment, and once started, must be continued for life.
While some people pay for these medications out of pocket, the majority of the costs are borne by insurance companies, employers, or other third-party payers. Currently, these drugs are covered by commercial carriers, as well as Medicare and Medicaid. As the popularity of these drugs continues to increase, the healthcare industry is looking at ways of reducing costs. According to KFF analysis of Centers for Medicare & Medicaid Services 2018-2022 Medicare Part D spending by drug increased from $57 Million to $5.7 Billion.[2]
The June 13, 2024 article in Fierce Healthcare[3] on GLP-1 drugs noted that Blue Cross Blue Shield of Michigan will no longer cover these drugs starting in January 2025, and will be changing the prior authorization criteria starting in August 2024, for those members that are in large group fully insured commercial plans. This raises the question of whether other payers will stop coverage and follow suit. Other considerations include if this class of medications is dropped from coverage, patients on the drugs will need to find other ways to pay for it if they want to continue, the affordability and availability of the medications, and what will the long-term impact be if patients stop taking the medications suddenly.
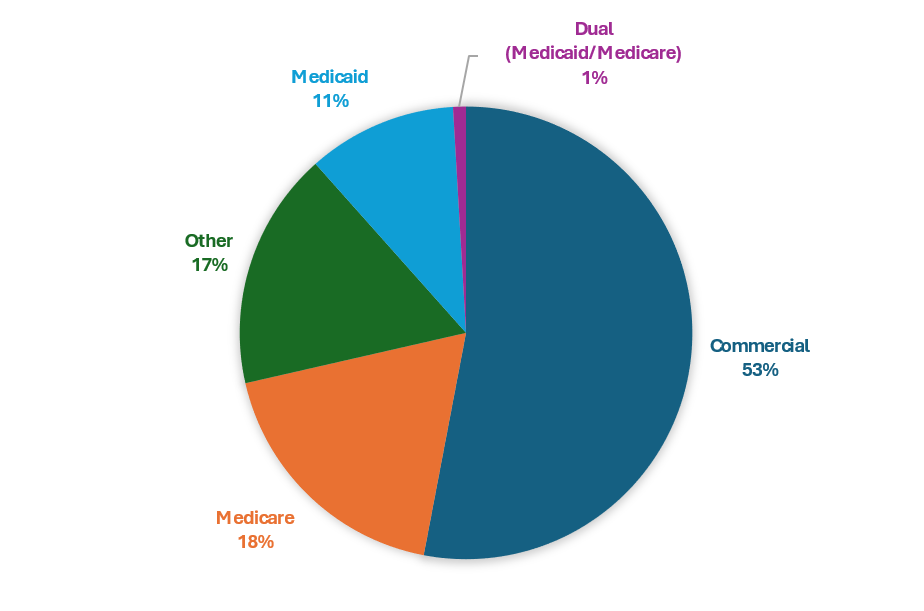
PurpleLab®, using its healthcare claims database and HealthNexus™ analytics platform, analyzed medical and pharmacy claims for 12.2M people taking GLP-1 medications from January 2019 – May 2024. In this population, 53% of individuals had commercial health insurance, 18% had Medicare, 11% had Medicaid, 1% had Dual (Medicare/Medicaid) coverage, and 17% had other coverage (e.g., Tricare, Veterans Affairs, or other State or local programs). Individuals receiving the medications through self-pay or other non-plan distribution channels were not included in this analysis. The medical and pharmacy claims are linked using Datavant tokens with Social Determinant of Health (SDOH) information derived from additional non-claim sources. When applying the filters for income, 56% of the patients taking a GLP-1 had income under $40,000, thus showing that patients in lower socio-economic classes can receive the medication if clinical criteria are met.
With the potential change in coverage, the out-of-pocket costs can be $12,000 a year or more to take these medications. For people in lower income brackets, this can have a profound impact on their lives. If the medications are discontinued, questions as to what the health ramifications to those individuals who cannot afford out-of-pocket coverage must be considered.
Given that our data show that more than half the patients taking GLP-1 medications earn less than $40,000 per year, this presents a financial challenge. How are individuals going to be able to afford these medications along with having to manage everyday expenses? Furthermore, what if employers that offer self-insured plans to their employees and dependents follow suit? If the individuals covered under these benefit designs no longer have access to the medications through their employers, many more individuals may have to make tough healthcare decisions.
Given that people may need to take medications long term, this raises not only financial and coverage determination questions, but it can affect physical health. GLP-1 have a positive impact on several cardiovascular risk factors such as obesity by promoting weight loss, blood pressure and blood lipid levels. Also, they stimulate the endothelium to produce nitric oxide, reduce oxidative stress, and have antiatherogenic and anti-inflammatory effects. [4] However, according to Harvard Health [5], there are potentially more serious side effects including pancreatitis, gastroparesis, bowel obstruction and gallstones. Over the next few years, we will need to monitor how the healthcare system will tackle these issues without the benefit of commercial managed care oversight.