Authored by: Russell Robbins, MD, MBA & Diane Faraone, Pharm D, PurpleLab™, Amy Pearlman, MSW, LICSW, Psych Hub
In the United States, mental healthcare resources have long been stretched thin. When the pandemic struck in 2019, there were more than 51 million Americans experiencing some type of mental illness. Pre-pandemic, many of these patients already struggled to receive the care they needed, and healthcare providers and facilities often lacked the resources to provide sufficient access to quality mental health care.
Unsurprisingly, the arrival of the pandemic only compounded these problems. Since 2020, living with the threat of contracting COVID-19 resulted in people existing in a constant undercurrent of fear. This reality not only exacerbated the symptoms of Americans with pre-existing mental health diagnoses, but it also increased the incidence of certain mental health-related symptoms.
Surging Demand for Mental Health Care Amid the Pandemic
From pre-COVID to the pandemic’s peak in 2020, the incidence of patients presenting with symptoms of anxiety and depression had more than tripled – from 11% to over 35%. Many of these patients were isolated from loved ones and missing out on essential social interactions and connections, which undoubtedly played a part in this unprecedented growth.
Before this point, the healthcare industry’s underlying infrastructure was already straining under the mental health burden in the United States. This infrastructure was ill-prepared to handle the impact of the pandemic. Simultaneously, there was rapid growth in the number of affected patients and the need to quickly stand up telehealth and telemedicine services. Additionally, the rise in anxiety and depression meant that the geographic distribution of this patient population had changed significantly.
With people seeking mental health care in new locations, telehealth services became even more critical for meeting this new demand. As a result, there was a decrease in face-to-face interactions in mental health care. This is a trend that has persisted, even as we emerge into a “post-pandemic” world. Although the arrival and distribution of COVID-19 vaccines have made it safer to return to in-person interactions, the widespread use of telehealth has persisted.
Navigating the Pandemic’s Lasting Impact on Mental Health Care
Two central issues emerged from the COVID-19 pandemic – a lack of qualified, licensed mental health professionals and growing demand for mental health care, particularly in rural and poorer areas in the US. The prevalence of mental illness has already decreased from its 2020 peak, but the impact the pandemic had on mental illness in the United States remains.
Now, in 2022, the incidence of depression and anxiety is estimated at approximately 30% – lower than that of a year ago but still higher than pre-pandemic levels. The pandemic increased an already chronic shortage of mental health providers, particularly psychiatrists. COVID-19 increased physical illness, overwork, and stress for healthcare workers across the U.S. In a field where work-related depression and anxiety were already rampant, these conditions inevitably resulted in widespread burnout throughout the nation’s healthcare workforce.
One 2022 survey reports that up to 47% of healthcare workers plan to leave the field by 2025. As more mental healthcare workers leave the field due to burnout, the increased incidence of depression, anxiety, and other mental illness creates the perfect storm for a mental health crisis on a national level. The remaining healthcare workers are asked to do more in terms of behavioral health. The overextended health system in the U.S. cannot fulfill the needs of patients living with mental illness, creating an environment where clinically emerging mental health conditions are more unlikely to receive the appropriate level and quality of care.
Examining the State of Depression and Anxiety Treatment Today
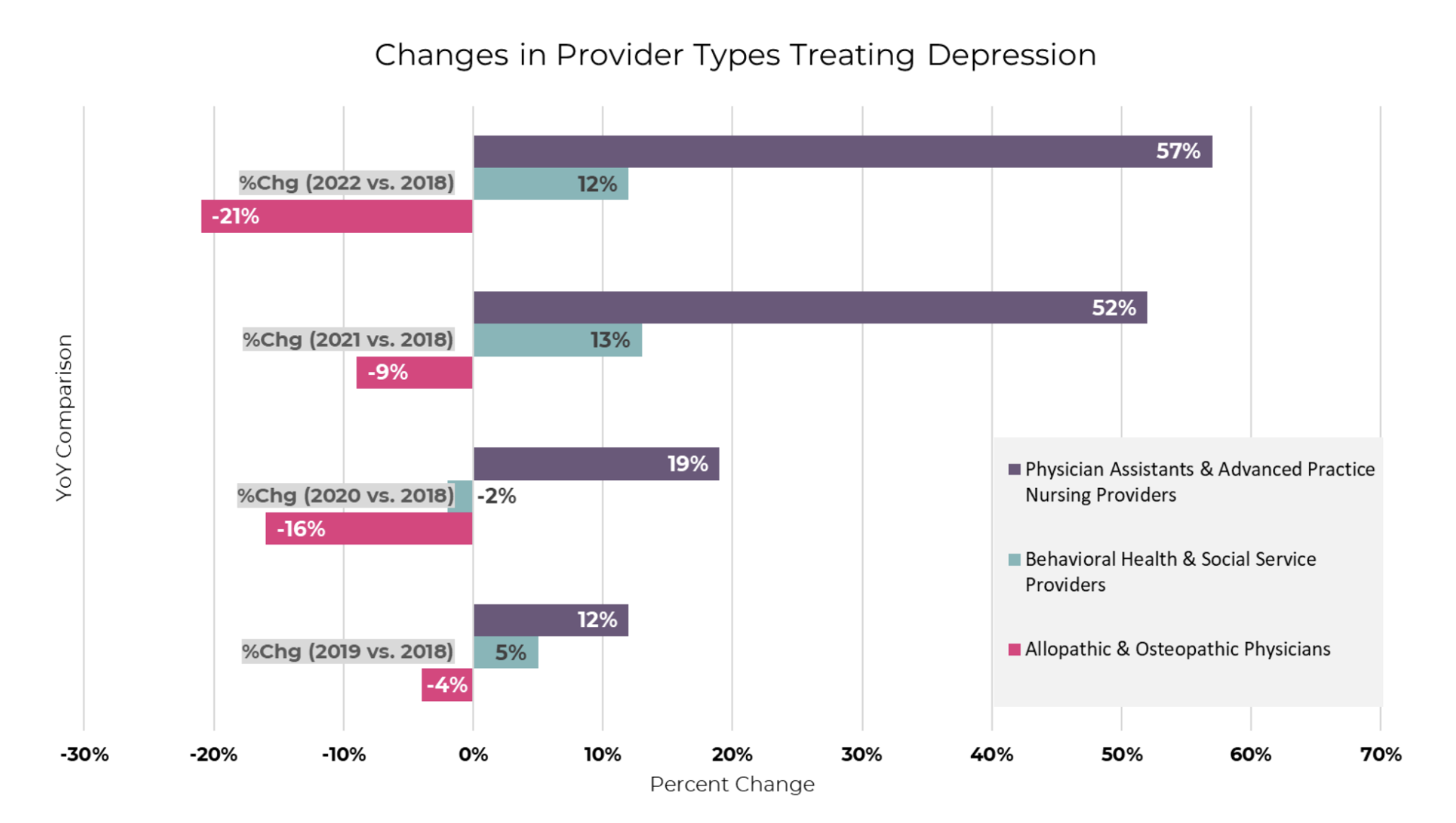
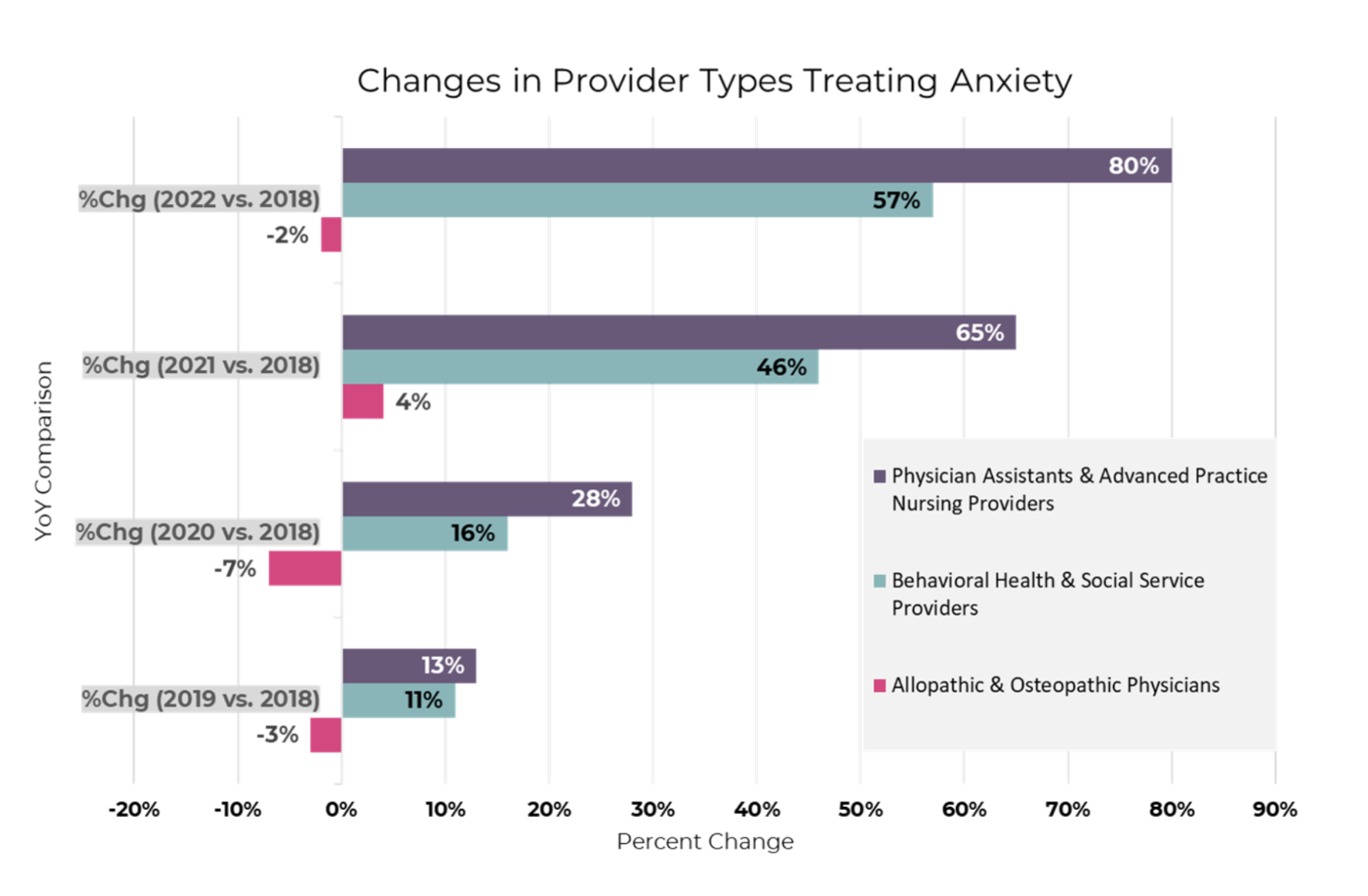
Using PurpleLab™’s HealthNexus™™ platform, we examined the availability of care for depression and anxiety using historical data on provider types treating these conditions, which included physician assistant and advanced practice nursing providers, behavioral health and social service providers, and allopathic and osteopathic physicians.
From 2018 to 2022, the data shows a consistent and potentially worrying shift. During this period, the percentage of behavioral health and social service providers treating depression and anxiety grew by 57% and 80% respectively. Even more striking, there was a compensatory shift from physician providers to extended care providers like physician assistants and advanced practice nursing providers.
For example, while the percent change in physicians treating depression was -21% from 2018 to 2022, the percent change for extended care providers was 12%. This pattern persists through all the findings in the charts shown below, although the percent change in physicians and extended care providers treated anxiety was much smaller.
Access to this type of information can help providers expand practices to address gaps in mental health care. Using available clinical data and social determinants of health (SDOH) can allow providers to gain insight into the prevalence and distribution of depression and anxiety disorders. Additionally, examining historical data from the COVID-19 pandemic can reveal provider- and location-specific impacts of the pandemic, insights that can then be used for emergency resource planning.
When we look at the changes in access to care as a result of the pandemic, we observe that patients and their providers were more willing to have telehealth services. While there was a decline in utilization after the peak of the pandemic, many of these changes persisted. As the prevalence of depression and anxiety remains elevated, it is critical that patients have better access to treatment from qualified providers.
This is just one example of how real-world data (RWD) can provide insights into important trends in provider specialty and treatment rates. PurpleLab™ and organizations like Psych Hub have created many solutions to identify, address and correct these problems. Using RWD analytics, providers can better identify and analyze potential gaps in care, allowing them to take action to mitigate the downstream illnesses that can result from a lack of access to quality care.
Contact us to learn more about HealthNexus™ powered by PurpleLab™ and to see how our platform can help you manage and use your healthcare data.