November 14th is World Diabetes Day, a day that many in healthcare use to highlight the challenges facing people living with diabetes, as well as the providers and organizations treating those patients. Established by the World Health Organization (WHO) in 1991, this global awareness campaign has served as a reminder of the need for increased awareness, education, and accessible care for people living with diabetes.
This year’s theme, “Access to Diabetes Care,” is especially timely. In the aftermath of the COVID-19 pandemic, healthcare providers (HCPs) and organizations (HCOs) worldwide are more aware than ever of the gap between the care available and the care diabetic patients actually receive.
Today, more than 130 million adults in the United States are dealing with the health consequences of living with prediabetes and diabetes. As the number of patients impacted by this disease continues to increase, improving access to diabetes care will only become more challenging.
Access to Diabetes Remains Challenging for HCPs and HCOs
This chronic disease is estimated to impact 1 in 10 adults worldwide – which equates to more than 523 million people. Many diabetics remain undiagnosed, which increases the risk to their quality of life and longevity. Over the past 30 years, World Diabetes Day has been an opportunity to call for increased awareness, education, and access to care for diabetes.
To manage their condition effectively – and minimize complications – diabetic patients need ongoing support from primary and specialty care providers, nurses, dieticians, and more. Given the strides made in remote monitoring and virtual health care during the last few years, patients with diabetes should theoretically have ready access to the care they need.
Unfortunately, that is not the case, and many healthcare organizations still struggle to effectively care for, educate, and support patients with diabetes, whether diagnosed or undiagnosed.
Diabetic Patients Face Increased Risk of Other Chronic Illnesses
Diagnosing and educating patients living with diabetes is a critical public health concern because diabetes carries significant risk of long-term complications. All three diabetes subtypes – Type 1, Type 2, and gestational diabetes – are characterized by frequently having significantly elevated blood glucose levels.
In people with Type 1 diabetes, those elevated glucose levels occur because they are unable to produce adequate amounts of insulin and therefore cannot intake glucose into their cells. Those with Type 2 and gestational diabetes, on the other hand, are unable to use their own insulin due to impaired glucose tolerance (IGT) and insulin resistance.
Although gestational diabetes can be dangerous, this condition often resolves after pregnancy – at the population level, Type 2 diabetes poses a much larger threat. Roughly 90% of diabetic patients are living with Type 2 diabetes. These patients are at risk of serious chronic illness, including cardiovascular disease, hypertension, and stroke.
The longer a patient lives with uncontrolled diabetes, the more damage their elevated blood glucose levels can do to blood vessels and nerves throughout the body. The resulting neuropathy and blood vessel damage can result in kidney failure, blindness, and even vascular dementia.
Achieving Better Health Outcomes for Patients with Diabetes
While the list of potential complications is long, people living with diabetes are not consigned to poor health outcomes or a shortened lifespan. With proper health care and lifestyle modifications, diabetic patients can maintain healthy blood glucose levels long-term and avoid many of the serious complications that they are at risk of developing.
Behavioral changes such as diet, caloric intake, weight management, and activity play a significant role in delaying or preventing common diabetes complications like cardiovascular disease. Additionally, these lifestyle modifications can also prevent patients with prediabetes from developing Type 2 diabetes. At the same time, these changes can also help maintain healthy blood pressure and cholesterol levels.
For some patients, lifestyle modifications alone are not sufficient to keep blood glucose levels under control. Due to a combination of genetics and environment, some patients need to combine healthy behavior with non-insulin prescription medications such as metformin. This is why it’s essential for prediabetic and diabetic patients to have access to ongoing medical care and health monitoring.
A Call for Action: Increasing Diabetes Awareness and Education
Diabetes – and Type 2 diabetes in particular – is on the rise worldwide, making it more important than ever that the healthcare industry improve both quality of care and health outcomes for this population. According to the International Diabetes Federation (IDF):
- Diabetes is responsible for 6.7 million deaths annually.
- IGT, a risk factor for developing type 2 diabetes, affects 541 million adults.
- In the United States, diabetes prevalence is even higher – 1 in 7 adults (51 million) are living with the disease compared to 1 in 10 worldwide.
- The number of adults with diabetes in the US is projected to reach 57 million by 2030.
- In the US, 1 in 4 adults is living with undiagnosed diabetes, adding to the $415 billion the US already spends on diagnosed diabetes patients.
Even when diagnosed, this chronic disease is often incredibly difficult to manage, both from the patient and the provider perspective. A single patient may have to start, stop, and switch between multiple medications, diets, and other lifestyle modifications while managing their condition throughout their lifetime.
Navigating these changes can be even more difficult when the changes required come into conflict with cultural norms, an increasingly common challenge as diabetes prevalence crosses international boundaries. Additionally, this disease still holds stigma in many areas, both in the US and worldwide.
To ensure patients adhere to healthy behaviors and use their medication as prescribed, HCPs and HCOs need to consider awareness and education levels when communicating with and supporting their diabetic patients. As the population of diabetic patients continues to grow, so will the number of patients requiring non-insulin, anti-diabetes medications.
How PurpleLab™ Partners with PQA to Improve Diabetes Care
As with any care plan that centers on drug therapy, managing Type 2 diabetes with anti-diabetes drugs depends on medication adherence. To combat diabetes complications, HCOs and programs need the ability to track patient adherence from a quality measure perspective.
Organizations like Pharmacy Quality Alliance (PQA) maintain quality measures that evaluate health plan performance on the quality of care patients receive. Quality measures like those from PQA help HCOs design programs that ensure patients are taking these medications – such as anti-diabetes drugs – correctly as prescribed to successfully manage their condition.
PQA is an independent, non-profit, national quality organization dedicated to improving medication safety, adherence, and appropriate use. Their quality initiatives include measure development for health plan performance measurement, research, and education, all of which support better medication use and high-quality care for patients.
Among their many ongoing initiatives, PQA has partnered with PurpleLab™ to develop a composite measure for medication adherence for diabetes and related diseases such as hypertension and hyperlipidemia. This kind of measure provides important insights into medication access for patients with diabetes, which has real-world value for both patients and healthcare payers.
Why Quality Measures Matter – The Impact of Adherence In Context
To put the value of medication adherence measures in perspective, we can first examine a recent report from the Centers for Medicare & Medicaid Services (CMS).
The report’s findings show how increased adherence rates for diabetes, hypertension, and cholesterol medications resulted in significant savings for the CMS. Over a 5-year period, the CMS avoided spending between $27 billion and $46.6 billion in estimated healthcare costs for Medicare beneficiaries taking these medications.
In the future, HCOs can use PQA’s composite measure for diabetes, hypertension, and cholesterol medication adherence to design programs that improve health outcomes for the affected patient population.
Additionally, using a PQA composite measure that assesses the adherence rates for diabetes, hypertension, and cholesterol medications, PurpleLab™ used our HealthNexus™ platform to examine adherence rates across all lines of business using open and closed claims.
As the charts below show, for patients in commercial healthcare plans, we found that adherence was relatively similar between genders (a difference of less than 5 percentage points). At the same time, patients over the age of 51 had significantly higher adherence rates compared to those aged 50 and younger.
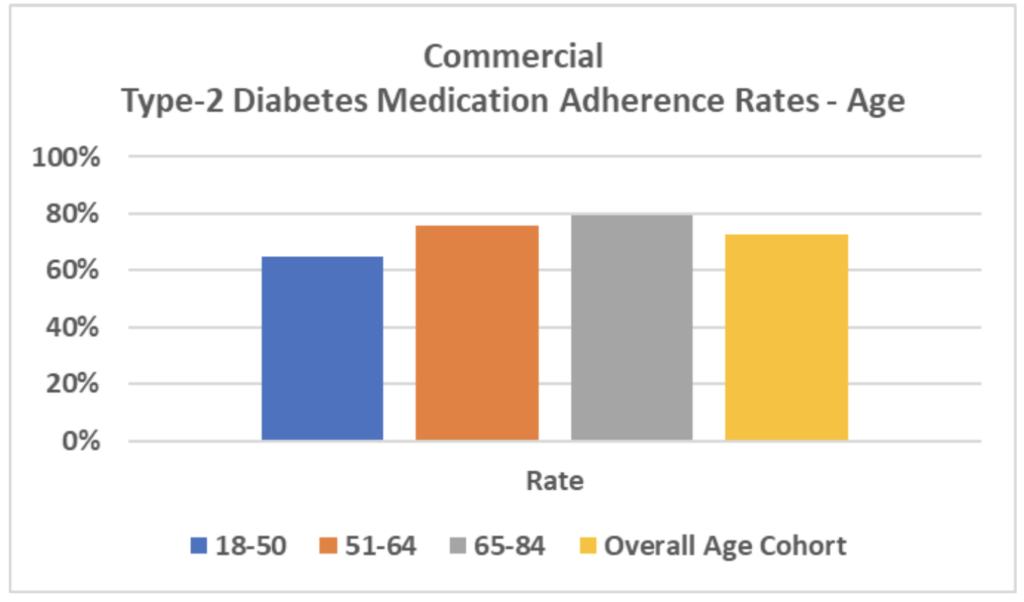
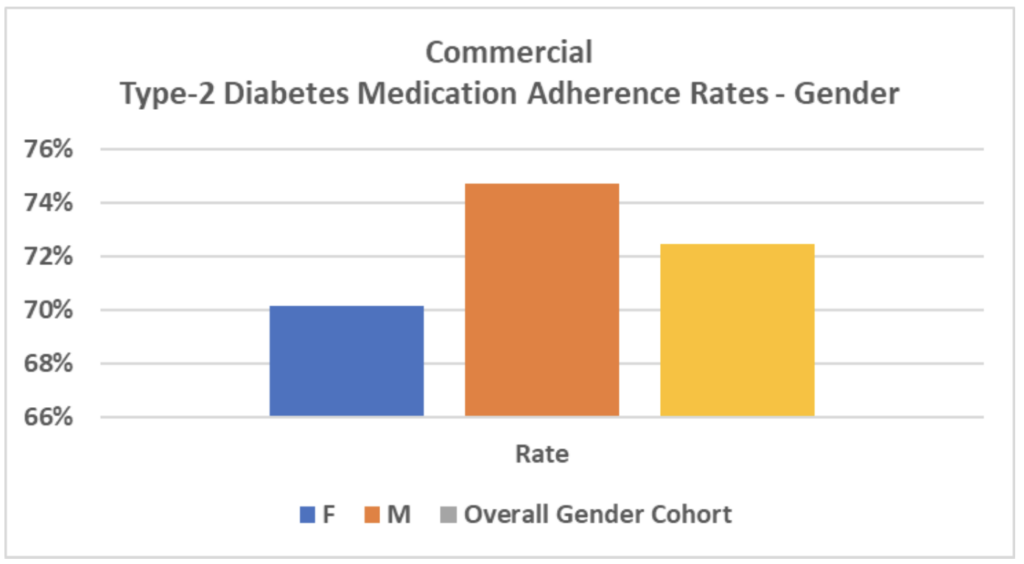
Understanding these dynamics is essential for improving diabetes care and health outcomes worldwide. Diabetes is not limited by age, gender, or socioeconomic status. By partnering with an organization like PQA, PurpleLab™ can use real-world data about new drug treatments and provider access to test quality measures that look at medication adherence as part of a holistic approach to preventing disease complications.
And by using quality measures, organizations can improve healthcare outcomes for at-risk patients, increase cost efficiencies, and better identify providers who know how to apply newer, more effective medication to treat diverse patient populations living with diabetes. Contact us to learn more about HealthNexus™ powered by PurpleLab™ and to see how our platform can help you manage and use your healthcare data.