PurpleLab® is driven by a singular goal – to provide healthcare organizations with robust and accessible real-world data (RWD) and real-world evidence (RWE) to solve conventional and emerging challenges, including tackling medication adherence. According to the FDA[1], real-world evidence (RWE) is defined as “the clinical evidence that looks at the usage and potential benefits or risks of a medical product derived from analysis of real-world data”. RWE can provide insights into patterns of medication use, adherence rates and factors affecting adherence.
According to the American Heart Association[2], poor medication adherence is associated with 125,000 American deaths annually and costs the healthcare system hundreds of billions of dollars every year. Medication nonadherence can lead to increased hospital admissions, stopped or delayed treatment, increased emergency room visits, and health complications which contribute to driving these staggering figures.
How can health plans continue to support their members in improving medication adherence to reduce these detrimental health outcomes and exorbitant costs? With real-world evidence (RWE).
A common but underutilized use case for RWE – health plans should leverage the data to identify patterns of adherence. Working with RWE helps plans to predict which members are at risk for poor compliance with their medications. Leveraging pharmacy and medical claims data provides a more comprehensive picture of their members, which helps to determine intervention strategies.
To create the most complete member profile, a plan must have access to data beyond its own claims. Adding robust open claims data, which provide information from a longer timeframe of the patient across multiple data sources and healthcare settings, enhances a plan’s understanding of its members. These illustrations[3] from the Journal of Health Economics Outcomes Research (JHEOR) show the difference between open and closed claims.
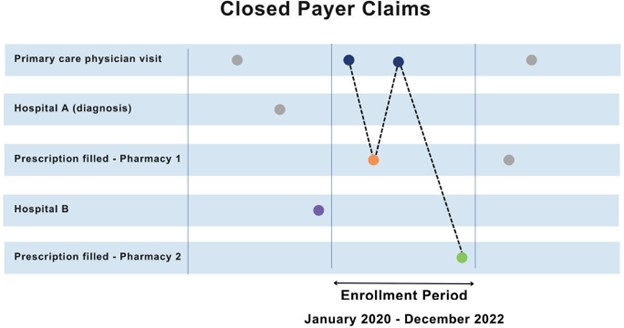
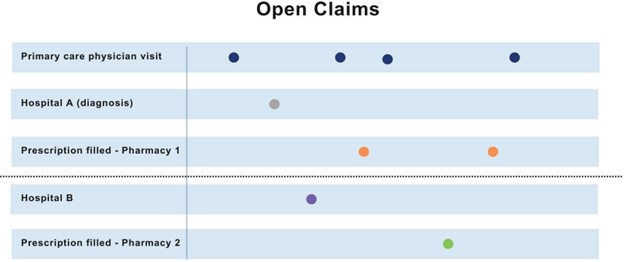
Why does this matter to health plan leaders? Greater visibility to claims data will help plans better manage their members and can help support improved medication adherence. According to JAMA Network[4], about 20% of commercial health plan members disenrolled from their plans each year. When this occurs, the health plan with only closed claims data would have a limited view of claims. Although members may come and go, chronic diseases do not. Therefore, without open claims providing a broader perspective, the plan may not have visibility to identify trends and issues needing to be addressed.
PurpleLab® can augment payers’ claims data to increase visibility and understanding of the lives they manage. Learn more about filling your claims data gaps to help you plan better, manage your members, improve medication adherence, and reduce the cost of care.
[1] https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence
[2] https://www.heart.org/en/health-topics/consumer-healthcare/medication-information/medication-adherence-taking-your-meds-as-directed#:~:text=Poor%20medication%20adherence%20takes%20the,emergency%20department%20visits%20and%20hospitalizations.
[3] https://jheor.org/article/87538-use-of-open-claims-vs-closed-claims-in-health-outcomes-research
[4] https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2789399