Osteoporosis and low bone mass affect almost 54 million people in the US, placing them at risk for hip, spine, wrist fractures, permanent pain, limited mobility, and increased morbidity and mortality. The disease affects people of all races, ethnicities, and gender, although significant variation within these groups does exist. For the over fifty population, osteoporosis affects one in five women compared to one in twenty men. A higher rate of osteoporosis and osteopenia in women is due to hormonal changes that occur after menopause, smaller bone diameter, and earlier bone resorption. Therefore, most hip fractures and injuries resulting from falls is significantly higher in women. Interestingly, osteoporosis and osteopenia may be underestimated in men, and although the disease presents less burden, they are still at risk.
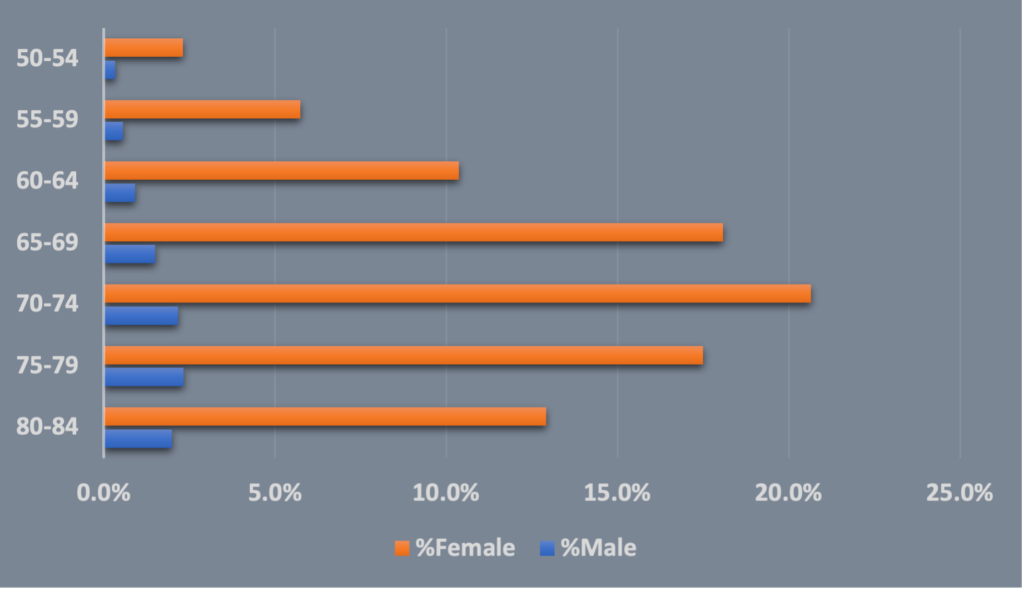
PurpleLab’s HealthNexus™ platform Cohort Report identified patients 50 years and older diagnosed with osteoporosis over a 5-year period. As data in suggests, (Figure 1), women are significantly more affected than men.
Fig 1. Osteoporosis patient cohort distribution by age and gender
What is Osteoporosis?
Osteoporosis is a condition caused by a decrease in bone mineral density (BMD), or bone mass. The incidence of developing osteoporosis is related to the amount of bone mass a person acquires when peak is reached, about age 30; the more accrued early in life, the lower the risk of developing low bone mass and osteoporosis. Bone is living tissue in a constant cycle of breakdown and renewal. Osteoporosis occurs when the body can no longer rebuild and replace old bone, leading to significant loss, reduced density, and weakened bones. Symptoms of early bone loss are non-specific, such as back pain, making it difficult to catch early. The first indication for most people affected is an initial bone fracture. Studies suggest the risk of breaking a bone due to osteoporosis in people over the age of fifty is one in two for women and one in 4 to 5 for men. For women who had an initial bone fracture, ten percent go on to have a second bone fracture within a year, 18% within the second year, and 31% within 5 years. These events often result in long-term or nursing home care. Sadly, up to twenty percent of seniors who suffer a hip fracture die within a year, typically from complications of the fracture itself or from surgery to repair the joint. The economic burden of osteoporosis has reached $19 billion a year with estimates the disease will cost upwards of $25 billion by 2025.
Other complications of osteoporosis and low bone mass are:
- Permanent pain
- Loss of height
- Stooped posture
- Limited mobility
- Isolation
- Depression
Who is at Risk?
Risk factors for developing osteoporosis are divided into three categories.
- Non-modifiable risk factors include female gender, advanced age, smaller body size, Caucasian and Asian race, family history, being post-menopausal as well as other conditions that lower estrogen and testosterone levels.
- Modifiable risk factors include diet and lifestyle.
- Diets low in calcium, vitamin D, and protein can increase the risk.
- Low levels of physical activity, heavy alcohol intake, and smoking can contribute to bone loss.
- Long-term use of certain medications such as corticosteroids, proton-pump inhibitors for reflux, and certain seizure and cancer medications can accelerate bone loss.
- Medical conditions that affect hormone levels, inflammatory bowel disease, rheumatoid arthritis, certain types of cancer, and diseases that lower the immune system, e.g., HIV/AIDS contribute to risk, but have the potential to be effectively managed
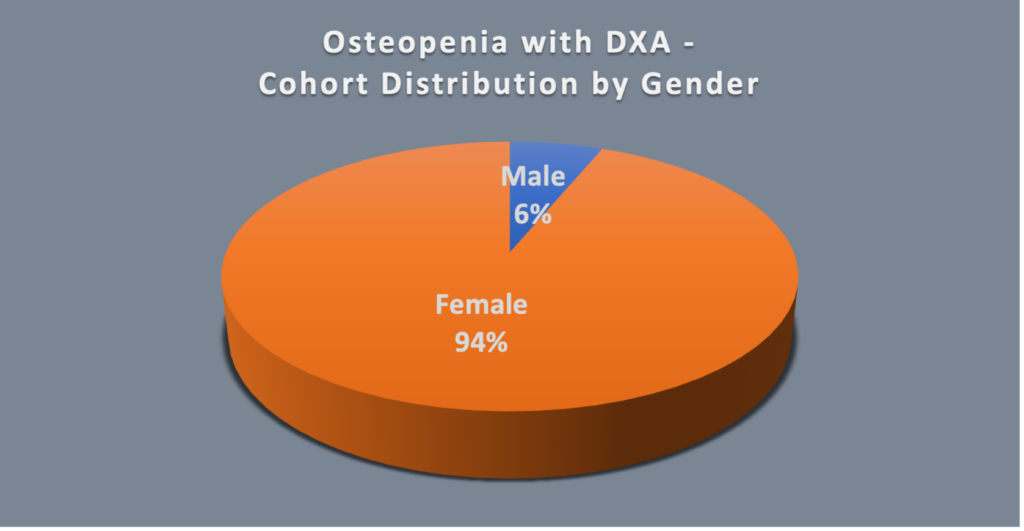
Osteopenia: A Precursor to Osteoporosis
There are also varying degrees of bone loss. About half of the population over 50 years has osteopenia, which is a midpoint between normal bone density and osteoporosis. The most accurate way to determine bone density is to have your provider order a DXA (dual-energy x-ray absorptiometry) test. This is a tool that is noninvasive and indicates level of bone loss as normal, osteopenia or osteoporosis using a T-score. This test is also used to evaluate whether osteoporosis treatment is working. The Bone Health & Osteoporosis Foundation (BHOF) recommends DXA testing for women 65 and older, men 70 years and older, younger men and women with risk factors, and those younger than 50 who have already had a fracture. Although the above recommendations are similar across gender only a small number of men undergo DXA screening (Figure 2).
Fig 2. Osteopenia patient cohort who underwent DXA and radiographic screening by age and gender
Prevention and Treatment
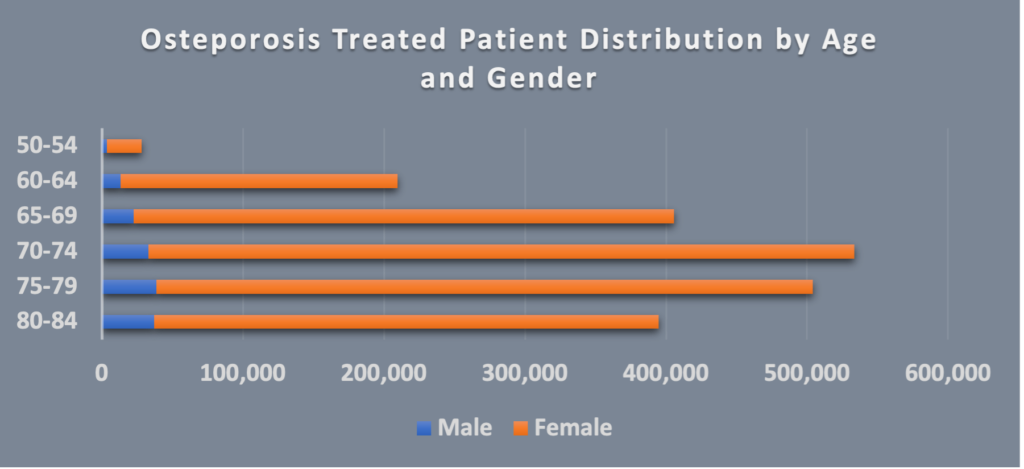
Preventing bone loss begins early in life and becomes more important as people age. This includes exercise, eating a nutritious diet high in calcium and vitamin D, not smoking, and limiting alcohol. If a healthy diet and active lifestyle are not enough to improve a low T-score, medication that focuses on preventing further bone loss such as a bisphosphonate along with vitamin D and calcium is the standard of care. Unfortunately, undertreatment of osteoporosis is something that exists across genders, however, this seems to be more of an issue in men as compared to women (Figure 3). Medication non-adherence to bisphosphonates is one of the proposed reasons for undertreatment.
Fig 3. Osteoporosis with treatment patient cohort
It is important for providers to engage, educate and inform their patients about treatment options and potential side effects as part of a shared decision process. Organizations such as 4BoneHealth and Healthy People 2030 are valuable resources for patients. 4BoneHealth provides education about prevention and treatment of osteoporosis and evidence-based information from experts in the bone health field. Healthy People 2030 focuses on preventing and treating osteoporosis. The collective goal is to increase screening and reduce the incidence of osteoporosis across the US population.
Having access to large quantities of data that can characterize and quantify patient populations for immediate insights, PurpleLab’s HealthNexus™ platform enables researchers the ability to create visualizations within minutes. Using defined medical and drug concept groups that leverage intersections of underlying and comorbid conditions with demographics and health variables, allows for an in depth understanding of patient populations. Please contact us to see how we can use our data to solve your healthcare needs.
https://www.osteoporosis.foundation/facts-statistics
https://www.nia.nih.gov/health/osteoporosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7924179/
https://www.osteoporosis.foundation/facts-statistics/key-statistic-for-north-america
https://www.bonehealthandosteoporosis.org/patients/what-is-osteoporosis/
https://www.bonehealthandosteoporosis.org/patients/diagnosis-information/bone-density-examtesting/
http://www.4bonehealth.org/category/whats-new/
https://health.gov/healthypeople/objectives-and-data/browse-objectives/osteoporosis