In 2019, the National Multiple Sclerosis Society published a series of findings with updated prevalence of the disease. Current estimates place the number of people diagnosed with Multiple Sclerosis (MS) at one million people in the US; double previously reported figures. It is a costly and chronic disease without an exact known cause or biomarker, although immune-mediated inflammation is thought to be a primary trigger. The diagnosis of MS relies on patient-reported symptoms, neurologic examination and imaging of the brain and spinal cord to detect areas of demyelination, called “lesions” that help to confirm presence and track progression of disease.
Most patients are initially diagnosed with MS between 20-50 years of age with a higher incidence in women compared to men. It is distributed across four subtypes: Clinically Isolated Syndrome (CIS), Relapsing-Remitting (RRMS), the most common form, Secondary Progressive (SPMS), and the most severe form, Primary Progressive (PPMS) occurring in 10-15% of patients at the time of diagnosis. PPMS is the ultimate course of disease after 20 years and is responsible for the greatest amount of disease-related neurologic disability, cost, and burden of illness. The total cost of care for MS is estimated at $85.4 billion, with $63B in direct costs including treatment and care and $22B in indirect and non-medical costs.
The American Academy of Neurology (AAN) best practices recommends that every patient diagnosed with clinically confirmed RRMS begin disease modifying therapy (DMT). These are oral, injectable and IV infusion monoclonal antibody and immunomodulatory medications that reduce disease relapses and delay neurologic progression. Because many patients with RRMS eventually progress to the secondary progressive form, initiating DMT early can improve symptoms, reduce disability, and lower that risk. Conversion to SPMS was also significantly lower for patients who received DMT mediations early versus later or not at all.
Deeper Insights with HealthNexus™ Cohort and Overlap Reporting Platform
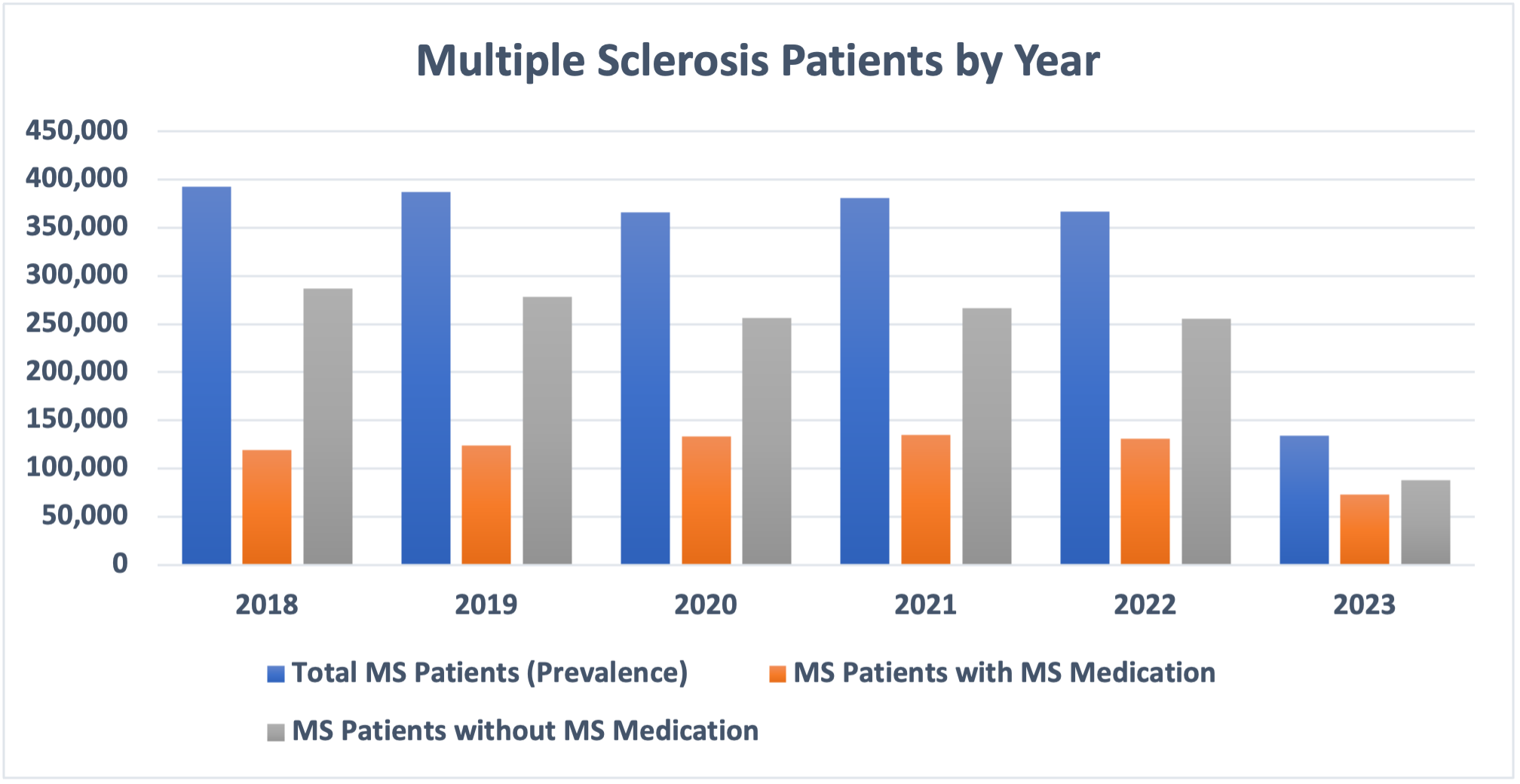
PurpleLab’s HealthNexus™ platform Cohort Report identified over 2 million people diagnosed with MS over a 5-year period. Interestingly, the percentage of patients without DMT was higher than those with DMT.
Fig 1. Multiple Sclerosis (MS) Patient Cohorts with and without Disease Modifying Therapy (DMT)
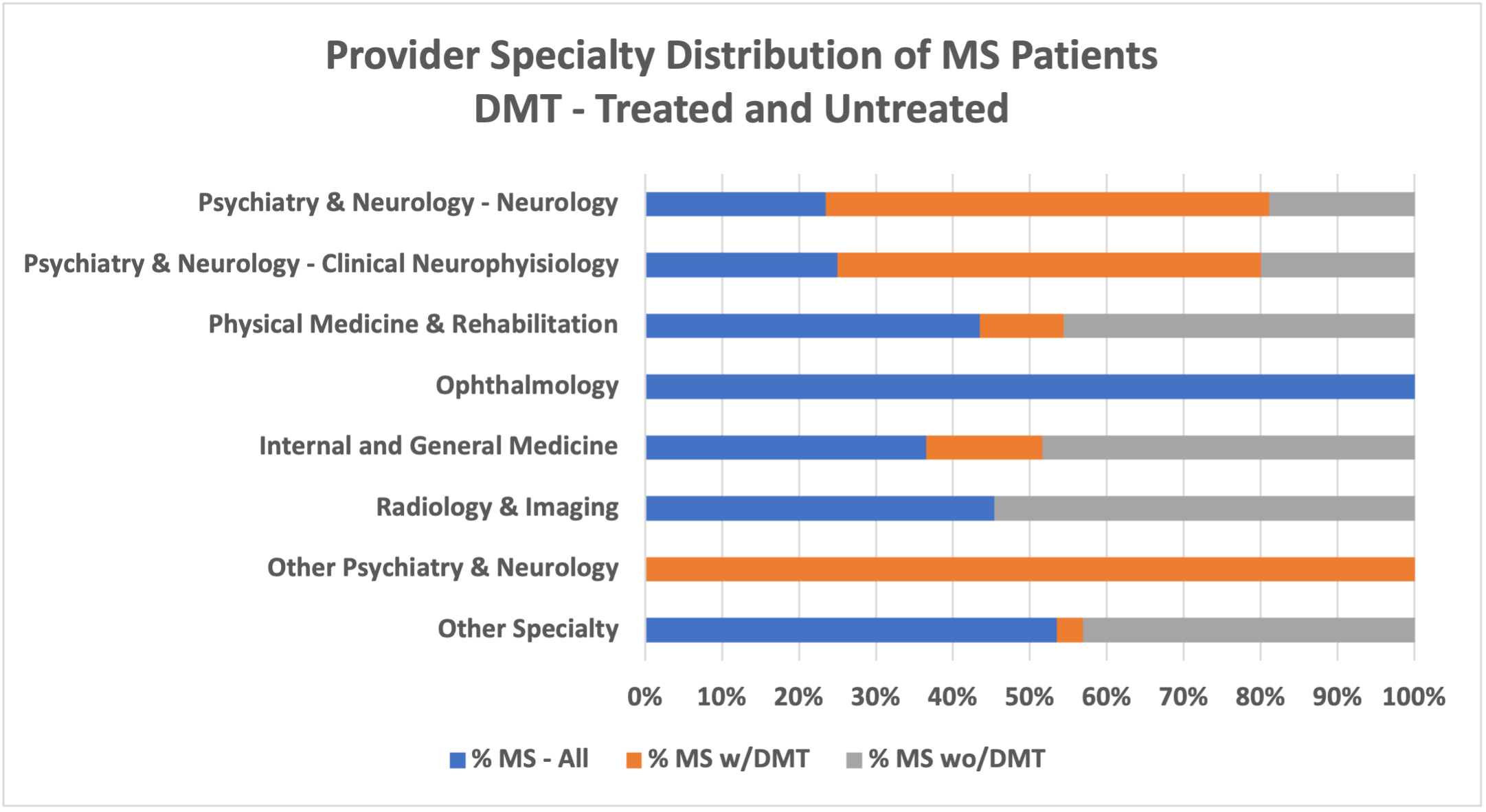
Further provider specialty analysis shows the distribution for overall care of MS is across many provider specialties with a higher percentage of internal medicine, general medicine, and psychiatry & neurology specialists. Considering DMT, compared to care for patients overall, those not on DMT received care from internal and general medicine specialists to a greater extent and fewer from neurology or neurology-related specialists. PurpleLab’s HealthNexus™ platform Overlap Report, Provider Type Summary, allows for a multidimensional analysis; each step builds the target disease and treatments of focus, with a distribution by provider specialty and sub-specialty taxonomy using defined medical and drug concept groups. The platform can help identify specific providers who have experience with diverse patient populations and providers who care for patients with complex therapy.
Fig 2. Healthcare Provider Specialty – Multiple Sclerosis (MS) with and without Disease Modifying Therapy (DMT)
Disease-modifying therapies (DMTs) reduce relapse rates and disease progression, but not all patients receive DMT. Patient-provider engagement impacts symptoms, relapse, and progression of disease in this population. MS symptoms may be vague or perceived as not severe enough. Patients that were engaged with providers during relapses had better information about issues related therapies, but even then, relapse follow-up across providers can vary. Other factors in DMT variation may be due to perceived lack of healthcare provider helpfulness and medication effectiveness and type of DMT medication that results in patients rarely or never engaging their healthcare provider during relapse. MS has more recently emerged as a chronic but manageable disease. Accurate diagnosis by a provider experienced caring for complex patients that applies best practices with early intervention can change the trajectory, and ultimately quality life of patients with this disease.
Patient and Provider Resources for Multiple Sclerosis Awareness Month
- National Multiple Sclerosis Society’s Pathways to Cures Roadmap had a mission to increase alignment and focus of resources, high priority research, and to inspire more collaboration that will accelerate scientific breakthroughs that lead to curing MS.
- National Neurological Condition Surveillance System (NNCSS) was authorized in 2016 as part of the 21st Century Cures Act, designed to track neurological conditions such as Multiple Sclerosis by continuous collection, analysis, and interpretation of health-related data that can be shared to inform and educate healthcare decision makers.
References
https://n.neurology.org/content/92/10/e1029
https://www.nationalmssociety.org/What-is-MS/What-Causes-MS
https://n.neurology.org/content/92/10/e1029
https://pubmed.ncbi.nlm.nih.gov/35418457/
https://n.neurology.org/content/90/17/777
https://multiplesclerosisnewstoday.com/treatments-that-modify-the-disease-course/
https://jamanetwork.com/journals/jama/fullarticle/2720726
https://journals.sagepub.com/doi/10.1177/13524585211010128
https://www.msard-journal.com/article/S2211-0348(18)30314-6/fulltext
https://www.nationalmssociety.org/pathways-to-cures
https://www.cdc.gov/surveillance/neurology/index.html