While only half as many are diagnosed, researchers estimate that hypothyroidism affects as much as 10% of the general population. Also known as “underactive thyroid,” this condition is characterized by a thyroid gland that doesn’t produce enough thyroid hormone (TH).
Hypothyroidism can have severe and lasting effects on a patient’s health due to the central role that the thyroid gland plays in regulating multiple organ systems throughout the body. The thyroid’s normal function is essential in maintaining healthy metabolic function. TH controls a number of metabolic processes, including:
- Inducing the breakdown or synthesis of macronutrients, such as proteins, fats, or carbohydrates.
- Bone growth and brain development through childhood and into early adulthood.
- Increasing the development of type II or fast-twitch muscle fibers, responsible for explosive movements.
- Stimulating increased perfusion or blood flow to the lungs, thereby increasing the lungs’ capacity for oxygen intake.
- Regulating cardiac output or the rate of blood flow out of the heart by increasing or decreasing heart rate, stroke volume, and contractility.
How Does Hypothyroidism Affect Long-term Health Outcomes?
In simple terms, TH is the end of a consecutive chain of hormones produced in the brain, serving as the interface between the endocrine system and many other organ systems.
Without sufficient TH levels released from the thyroid gland, many processes related to growth, cellular repair, and oxygen delivery are interrupted. Untreated, the effect of this condition can be devastating to patients’ quality of life and expected lifespan.
While severe hypothyroidism is uncommon, even those with moderate TH deficiency can experience:
- Compromised immunity and increased risk of infection.
- Reproductive issues, including infertility, miscarriage, and birth defects.
- High levels of LDL cholesterol, heart disease, and even heart failure.
Globally, hypothyroidism is most commonly caused by iodine deficiency. Since the introduction of iodized salt, however, most patients in developed countries are unlikely to lack sufficient iodine in their diet. So when patients are showing multiple signs of hypothyroidism – such as tiredness, cold sensitivity, muscle weakness, thinning hair, and slowed heart rate, among others – it’s important that they are tested for low TH levels.
Among those with sufficient iodine intake, the vast majority of patients with low TH levels have what’s known as primary hypothyroidism, a condition in which TH levels are low due to the destruction or removal of the thyroid gland. Less than 5% have secondary hyperthyroidism, which is caused by a deficiency in thyroid-stimulating hormone (TSH).
Why Hypothyroidism Is Both Simple and Difficult to Diagnose
The diagnostic procedure and criteria for hypothyroidism are fairly straightforward. In cases of suspected hypothyroidism, physicians first test patients’ TSH levels. If TSH levels are higher than the reference range (i.e., the upper and lower limits of values seen in healthy adults), they then test for low TH levels to confirm a diagnosis of primary hypothyroidism. If both TSH and TH levels are low, the patient likely has secondary hypothyroidism.
The problem is, despite the thyroid gland’s global influence on the body’s metabolic process, during early stages of hypothyroidism, patients often don’t experience or notice its symptoms. It’s important for healthcare providers to proactively recognize when patients repeatedly report ongoing symptoms that match this disease profile, especially among patients that exhibit multiple risk factors.
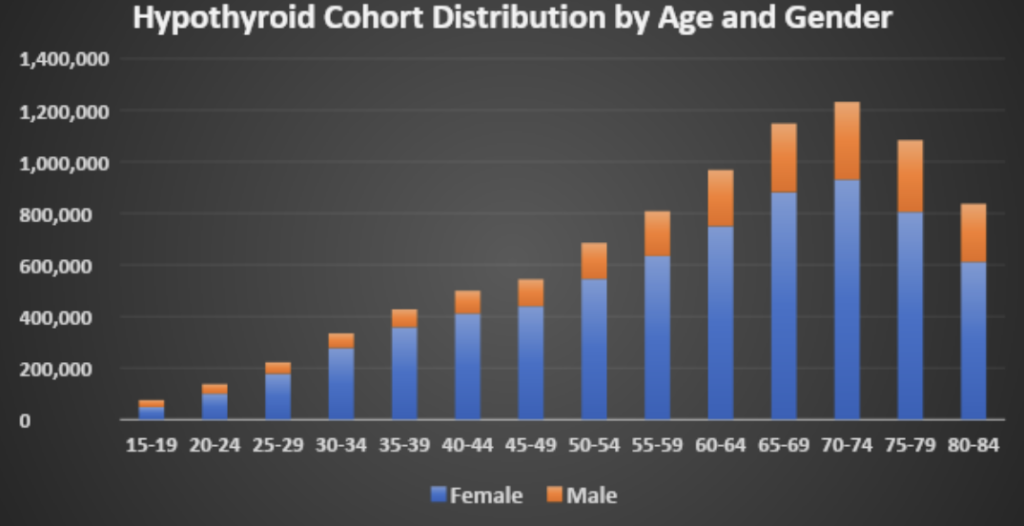
For example, thyroid problems are significantly more common in women and the rate of hypothyroidism increases with age for both men and women, as evidenced by the data from PurpleLab’s HealthNexus.
Supporting Patients with Hypothyroidism
Due to lack of education or awareness, undiagnosed patients are often unaware that the symptoms they’re experiencing are attributable to hypothyroidism. Additionally, TSH and TH blood tests are rarely included in preventative lab work. Ensuring patient-facing providers are asking the right questions and noting trends in reported symptoms indicated of this condition can go a long way to reducing its long-term health consequences.
Whether patients have had their thyroid gland damaged or removed due to prior treatment (e.g., surgery or radiation), the gland was destroyed due to an autoimmune disorder (e.g., Hashimoto’s disease), or they produce low levels of TSH, the recommended course of treatment is generally the same.
Patients with clinically detectable primary or secondary hypothyroidism have to take daily doses of levothyroxine, a synthetic TH replacement. Because the drug mimics naturally occurring TH, taking levothyroxine can reverse many of the negative symptoms patients experience with low TH and can have little to no harmful side effects if TH levels remain within healthy ranges.
But having too much TH in the bloodstream can also have serious consequences, including loss of bone mass (which can worsen and become osteoporosis) or dangerous heart arrhythmias. As such it’s equally important that these patients are properly diagnosed and monitored over time.
Notably, many women’s supplements contain biotin, which can interfere with the actual measurement of TH. To ensure that thyroid status is accurately reflected, supplements containing biotin should be stopped at least a week before having thyroid blood work checked.
Contact us to learn more about HealthNexus™ powered by PurpleLab™ and to see how our platform can help you manage and use your healthcare data.